A heart can be no more forced to love than a stomach can be forced to digest food by persuasion.
– Alfred Nobel
Read time: 15 minutes
TL;DR Key Points:
- Bloating is the uncomfortable perception of gas.
- Bloating is primarily an issue of gas handling by the gut and less often of excessive gas production
- Kombucha will not heal your gut no matter what the person at Whole Foods tells you
Disclaimer: This is NOT to be taken as professional medical advice to diagnose, treat, or manage any medical complaints. This is solely for general education. Please consult your healthcare practitioner regarding your particular concerns. No liability will be held regarding this essay or any content on this website.
“Carb coma.”
“Food baby.”
“I can’t fit into my jeans even though I haven’t gained any weight!”
“ I look like 6 months pregnant.”
“My stomach used to be flat. Now it’s like this”

I hear some version of these comments from patients almost on a daily basis. It seems to be an epidemic. So what’s going on? And what can we do about it? Read on, my friend!
What actually is bloating?
Bloating is the uncomfortable awareness and sensation of abdominal pressure. It is important to realize that everyone feels this from time to time. Bloating is a normal physiological function in response to a meal and a part of life. How else could we eat otherwise?
Expectations of eliminating all bloating are unrealistic and not healthy. Rather, we should strive to minimize excessive bloating and learn to become comfortable with normal bloating sensations without trigger anxiety or distress.
However, the recurrent or chronic nature of these complaints is when it becomes pathological and merits some investigation. As you can imagine, to a certain degree this is a matter of individual perception and so is a bit of a moving target.
Note that bloating is not the same as abdominal distention. You can have one without the other. The latter refers to physical enlargement of the abdomen, i.e. visible enlargement of the waist. Similarly, either burping or flatulence often but not always accompanies bloating.
Bloating can be mistaken for a variety of things including ascites (seen in liver and heart disease especially), fat (either visceral or subcutaneous), protein wasting (seen in malnourished children in developing countries, in particular). Bloating can also be confused for abdominal fat – either beneath the skin or around the abdominal organs.
The Usual Suspects
Many organic problems can cause bloating, like ulcers or bowel blockages. Other potential considerations:
- GI infections
- Nutrient malabsorption problems (eg Celiac disease)
- Significant Heart and Liver Disease
- Changes in blood flow to the intestines
- Bowel blockages
- Inflammatory Bowel Disease (eg Crohn’s, Colitis)
- Gynecological concerns: altered menstruation, female hormone dysfunction
- Autoimmune conditions: Lupus, Rheumatoid Arthritis
- Colon cancer
If these issues are not present then we consider an evaluation for functional bloating. Practically, speaking most people who complain of persistent bloating fall into this category.
Physiologically, problematic bloating of this sort comes from nervous system dysfunction of the gut and poor motility, inappropriate handling of gas and fluid and intestinal inflammation. Specifically,
- Brain Gut Axis – The gut acts a “second brain,” given the large number of nerves and neurotransmitters it helps produce. Alterations in brain gut signaling can create distressful bloating. Read more here.
- Altered Intestinal Bacteria – Prior GI infections, SIBO (small intestinal bacterial overgrowth), antibiotics, and the potential role of probiotics all fall in this category. The numerous bacteria that reside in our gut directly influence our health. When it is disturbed, GI dysfunction can result.
- Visceral Hypersensitivity – For reasons still unclear, patients with functional bloating are often more sensitive to pain and internal stimuli that the rest of us. This may occur through neurological changes in local receptors or in how the brain reacts and processes these pain signals. At the level of the brain, emotion and gut distress and pain are deeply intertwined. The role of stress, anxiety and other emotions is key. Here, patients can have an exaggerated response to even normal intestinal stimuli.
- Food sensitivities – Note this is not the same as “food allergies,” which is an overused term and is actually quite rare as a practical matter.
- Intestinal Motility Problems –Motility refers to the process of the nerves and smooth muscle of the gut coordinating together to manage nutrients. How do our guts handle internal stimuli and move things along? Problems here are common in patients with bloating, IBS and similar challenges.
- Intestinal Inflammation– Low grade intestinal inflammation can create disrupt the lining of the gut and create a cascade of molecules that can impair the handling of foodstuff, digestive enzymes, waste and gas. The Internet has dramatically overemphasized this factor in order to gain headlines (“Everyone has leaky gut!”)
- Inappropriate use of your diaphragm – the diaphragm is the top bookend of the abdominal cavity. Using this muscle inappropriately can cause prompt bloating due to muscular imbalances and poor coordination with the diaphragm (so called “dyssynergia.”)
- Hormones – Women know this better than men because it is not uncommon for them to get bloated during their menstrual periods.
A visual representation:
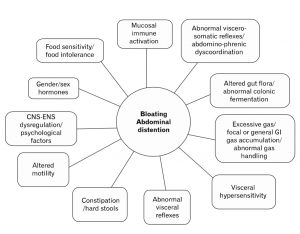
In other words, what you eat is essential but NOT the only factor involved in bloating.
Let’s address a few of these in more detail.
Air and other Gases
Aerophagia means literally eating air. Rapid eating (an epidemic in our on-the-go lifestyle), use of carbonated beverages and artificially sweetened gums and desserts are all common causes of this problem.
Having said that, this tends to be a minor cause of bloating because normally the intestinal wall is able to expel various gases easily (N2) and absorb others through diffusion easily (CO2, O2). Moreover, aerophagics tend to belch quite a bit also.
But if you find yourself burping a lot, try slowing down (you’ll enjoy your food better), and limit some of these trigger items.
Food
Highly fatty foods and certain carbohydrates tend to alter the balance between the volume of our innards and the resting tone of the muscles lining them. Some fermentable foods like beans and some fruits and veggies can increase water retention and gas production in the small bowel as well as shift local blood flow. These are called FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols) and hence the rising popularity of the low FODMAP diet.
Gas & Bacteria
If not a direct response to external stimuli (air, food) bloating can be a response to internal stimuli. In fact, the two major organ systems in our bodies that bridge the outside world and our inner environments are the gut and the skin. Hence, perhaps it’s not surprising their biological structures are similar and we can see problems in one pop up in the other.
Fermentation of dietary and endogenous (created by our body) substances can cause discomfort. 70% of gas produced is in the colon but only a quarter of this is expelled from the anus, meaning that upward migration of gases (CO2, H2, CH4) is common. This gas retention can cause that uncomfortable sensation we all know too well.
Having said this, the normal GI tract has approximately 100ml of gas and this is NOT typically increased in chronic bloaters. Rather, it tends to be inappropriate handling of gas that causes much bloating.
SIBO, or small intestinal bacterial overgrowth, falls into this category. For a variety of reasons (diet, anatomy, surgery, antibiotics etc.) we will discuss in the future, some patients can develop excessive bacteria in the mid gut. These players are often gas producing (H2 and Methane, as a practical matter) that can cause a whole host of gut complaints for individuals.
Bodywork
In some patients, bloating can be aggravated by abnormal lumbro-sacral (lower spine) and pelvic relationships, tight hip flexors and weak core muscles due to our poor movement patterns. This can worsen troublesome breathing habits (see below) and inappropriate use of our abdominal and breathing muscles.
Tension in one part of the body tends to travel and spread to other parts.
This is a biomechanical truth (fascia connects our entire bodies together) as much as an emotional one (any actor has likely heard the dictum to relax to dissipate tension to improve their ability to be in the moments). Becoming more comfortable (literally) in your skin can improve bloating. Moreover, it can decrease some of the hyper vigilance that patients with pronounced bloating can have.
In psychodynamic world, trauma is often encoded into the body in various manners. Regardless of whether this is true, it can be useful to explore the concept with a practitioner to see if emotional hurts have been the source of unexplained tension in your body.
Physical exercise and core training are important factors in improving the transit time of expelling intestinal byproducts as well. This is a key part of active release therapy and other myofascial stimulatory practices.
Breathing
The quickest way to modulate your nervous system is to alter your breathing. As the Zen saying goes, when the breath is steady the mind is calm.
As previously mentioned, data shows that abnormal use of the diaphragm can prompt additional bloating through dysfunctional neural arcs. Normal individuals react to GI gas by contracting their anterior abdominal muscles and relaxing their diaphragm. In patients with bloating and distention, they have different reflexes that lead to thoracic expansions, diaphragm contraction and relaxation of their core muscles.
Appropriate breathing, so-called diaphragmatic breathing, can help correct this. It’s what those models on the cover of Yoga magazines are attempting to demonstrate.
Try the following exercises:
Diaphragmatic breathing technique
Lie on your back on a flat surface or in bed, with your knees bent and your head supported. You can use a pillow under your knees to support your legs. Place one hand on your upper chest and the other just below your rib cage. This will allow you to feel your diaphragm move as you breathe.

Breathe in slowly through your nose so that your stomach moves out against your hand. The hand on your chest should remain as still as possible.

Tighten your stomach muscles, letting them fall inward as you exhale through pursed lips. The hand on your upper chest must remain as still as possible.

Think: breath through your back. You should not have a significant lumbar extension. Using a straw to breath will make this exercises more challenging. You can try this sitting in a chair, or with your back on the floor and your feet propped up flat on an adjacent wall.
Note: You may notice an increased effort will be needed to use the diaphragm correctly. At first, you’ll probably get tired while doing this exercise. But keep at it, because with continued practice, diaphragmatic breathing will become easy and automatic.
Photo cred: Cleveland Clinic
Okay, okay so how do I feel better ?!
Easy Fixes:
- Slooooow doooowwwn your eating
- Minimize use of artificial sweeteners in low sugar foods like erythritol
- Decrease the total number of calories. Eat till 80% full – the Okinawan practice called hara hachi bu
- Ensure you’re going #2 regularly
- Chill. Chillax, even, if you’re feeling ambitious
- If you’re new to fiber (and most of us are in ‘Murica), then ease in to it. Otherwise , your gut is going to rebel like the hosts on Westworld
- Minimize greasy, highly processed foods, either carbs or fats (please, no angry emails Keto folk)
- Avoid abrupt changes in dietary habits to give your intestine time to acclimate (see a theme here?)
- Don’t obsess about your bloating
- Cut down on the alcohol.
- Get familiar with how to use a lacrosse or tennis ball and the process of myofascial release. Kelly Starrett of Mwod is a great resource
https://www.youtube.com/watch?v=9qdTxxxmCzc
A practical approach
- A food diary and consultation with a nutritionist.
- Psychological counseling and mental health support +/- medication
- Breathing training
- Bodywork
- If these don’t work, time to see a physician to see if other strategies (smart bacterial manipulation: antibiotics, probiotics, prebiotics, neuropathic medications or pro-motility agents) are valuable
Afterword: A comment about body image
In our Instagram world, body image preoccupations and anxieties have worsened. It can contribute to an inappropriate fixation on abdominal complaints and appearance. Unsatisfactory self-appearance of abdominal distention can trigger a vicious cycle of underlying stress/anxiety and depression. Resetting expectations and understanding what is actually normal versus abnormal is key to an improved quality of life.
References:
[1] Seo, AY and Oh DH. Abdominal Bloating: Pathophysiology and Treatment. J Neurogastroenterol Motil 2013;19:433-453.
[2] Cleveland Clinic, Diaphragmatic Breathing.